13th of July 2024
Orthopaedic surgical visit 11 March to 15 March 2024
In Tonga it is the rainy season during March and sure enough arriving early Monday afternoon on a Dreamliner Boeing 787, it was raining and continued to do so for most of the week. On arrival at Vaiola hospital I undertook an OPD clinic where 35 patients were assessed that afternoon. To assess that number, I was ably supported by four local doctors who gave a summary of the patient’s problems to me. Then they did all the transcribing after assessing the patient together with me. Having this assistance enabled me to teach, particularly the junior doctors and assess as many patients as we did.
The patients varied with multiple problems mainly fractures – old and new, infections, back problem, congenital problems, Osteoarthritis etc. During this clinic I was able to determine which cases were suitable for surgical intervention that were booked for the rest of the week. It was also a good clinic to assess those patients who I had operated from my previous visit last November.
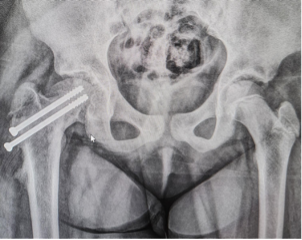
There was one girl who I was interested to review who had failure of fixation of her slipped upper femoral epiphysis (SUFE) right hip middle of last year. The complication was unusual in that the slip had improved because of her developing a painful pseudo (false) joint through a fracture that had occurred around the neck of her femur. The fracture was fixed with two screws (xray below) at my last visit in November and as this girl was large for her age, it was decided to bed rest her in traction for six weeks to ensure adequate healing rather than have a repeat of the previous fixation failure with her mobilising to early. On review at this clinic three months after surgery, it was good to see her walk normally and pain free.
This case illustrates the improvement in the Orthopaedic service in Tonga over recent years that has come about with the use of a trauma table being sent over to Tonga from New Zealand in 2021 and equipment purchased from India to allow for this form of fixation. It also shows how a potentially complex case can have an excellent outcome with a team approach.
There was a pleasant surprize during this clinic as I was given a gift from a patient who I had operated on during my last visit, for a fracture to his knee joint that required fixation.
The next four days were focused on surgery with some outpatient cases assessed before and between surgical cases.
Overall, it was a very productive visit. In total 50 patients were assessed clinically in the OPD, theatre suite and in the paediatric/surgical wards. There were ten DNA’s. Two patients were given cortisone injections in OPD. 12 patients were operated on.
In addition, I was able to have meetings to organise the upgrade of the operating theatres with the main stakeholders that has now been planned for later in the year. There were surgical cases that gave the resident surgeons the opportunity to undertake operations under supervision so they could be more confident to do these cases in the future. Also, I had the opportunity to plan for the rest of the year as two months will be set aside later in the year for the theatre upgrade, which means there was less options for visits because of the other visiting surgical teams. Unfortunately, I will only be able to visit once more this year in August but hopefully I will be the first to use the new operating theatres in January 2025.
Tuesday 12 March
The third operative case listed below was an excellent educational case of how to apply an external fixator onto a significant open fracture of the Tibia (Shin bone). The last case was of a neglected ankle fracture which had healed badly. The only way to improve the position was to break down the fractures on either side of the ankle joint and then as best as possible reduce it into an anatomic position. This is not the first time I have encountered such a case.
Earlier in the day I was also able to advise on two cases from the same family afflicted by Osteogenesis Imperfecta.
OPD cases
23 VH M 18 Osteogenesis Imperfecta – Lower back problem with scoliosis. Advice given.
24 LH F 19 Osteogenesis Imperfecta Dysplastic left hip joint. Advice given.
Surgical cases
O K M 12 Septic arthritis of the left hip joint. Rx Washout left hip joint Surgeons; JvD, Tu’ipuloto.
S M M 13 Sepsis – Right shoulder and elbow joints Rx Incision and drainage Surgeons; Tu’ipulotu, JvD.
E M M 11 Washout of wound and application of External fixator right Tibial fracture Surgeons; Tu’puloto and Aholeli. Supervisor JvD.
L W F 27 Old displaced AO type C fracture left ankle joint. Refracture and ORIF of displaced AO type C fracture. Surgeons; JvD, Aholeli.
Wednesday 13 March
On Wednesday it was a full surgical day with also a meeting with the procurement office personnel at mid-day to discuss finances for the upcoming operating theatre upgrade. The hope is that finances will now become available in the next few weeks to allow the contracting team Pharmac Tech to proceed with purchase of materials and commence with prefabrication.
The interesting case was the second case in which fixation of an old, displaced elbow fracture in a four-year-old boy was undertaken. To do this procedure required re-breakage of the fracture and fixation in a more anatomic position using K wires. If this elbow were left as it was, the child would have had significant problems in the future.
OPD
17 S F 37 Chronic osteomyelitis left mid foot. Rx Fluclox. Rifampicin unavailable. Refused surgical debridement. Rx Rifampicin and Fluclox.
44 U L F 37 Cortisone injection left carpal tunnel.
Surgical cases
16 ST F 75 Failure of fixation for intertrochanteric fracture right neck of femur. Removal of hardware right proximal femur. Surgeons; Aholei Supervisor JvD.
26 PH M 4 Old displaced right lateral condyle fracture. Refracture and ORIF with K wire fixation. Surgeons; JvD, Aholeli
52 TA F 26 ORIF of right LisFranc ligament injury. Surgeons; JvD, Tu’ipuloto.
31 SM M 64 ORIF of old subcapital fracture left neck of femur with cannulated screws. Surgeons; JvD, Aholeli.
Thursday 14 March
At 3.30 pm an important zoom meeting was held with Pharma Tech (India- Mangalore) and with the Tongan procurement office as well as with Drs Tangi and Akuola and me to discuss matters pertaining to the operating theatre upgrade project. The project had been delayed because of the Procurement office requirements for more information. Matters discussed were the finances, revised MOU, shipping of the container, accommodation for the visiting personnel from India and visas, flight tickets as well.
Later in the day I had a meeting with Semisi Fukofuka from the New Zealand High Commission to discuss support for the project.
The operative cases were interesting. The first and third cases I allowed Dr Aholelei to be the lead surgeon so she could gain more confidence with these procedures.
OPD
29 S T M 64 Diabetic peripheral neuropathy Rx Gabapentin.
54 M V F 76 Distal left radius fracture Rx Physio
T F F 47 Calcific tendonitis right shoulder Rx Conservative
Surgical cases
28 PH M 16 ORIF Right SUFE Surgeons; JvD, Aholelei.
37 LC M 15 ORIF of displaced left radius and ulnar. Surgeons; JvD, Aholelei.
16 TM M 75 ORIF of hypertrophic fracture right neck of femur. Surgeons; Aholelei, JvD.
Friday 15 March
I was able to have a further meeting with Sami Mafile’o, from the procurement office to organize an action plan for the operating theatre project following the zoom meeting with the main stakeholders the previous afternoon.
I allowed Dr Aholelei to undertake a SUFE case by herself with some instructions given during the mid portion of the surgery.
OPD
TF F 47 Cortisone injection left shoulder for calcific tendonitis.
Surgical case
ORIF of right SUFE Surgeons; Aholelei, JvD Supervisor.
I flew out at 2.50 pm for Auckland, arriving on schedule, allowing me to catch an earlier flight to Palmerston North at 7.30 pm to be home that evening.
John van Dalen 19 March 2024